ParaRev has received several questions regarding coding for colonoscopies. The following Q&A will help provide clarity on the use of modifiers, E/M coding and medical necessity.
Q | We have been working with our coders to better help them understand modifiers XS and XU. When reporting two or more diagnostic colonoscopy codes, is it appropriate to append modifier XS (separate structure), or should we report modifier XU (unusual, non-overlapping service)? For example, we need to append a modifier to report 45380 with 45385 to resolve a CCI edit. | |||||||||||||||||||||||||||
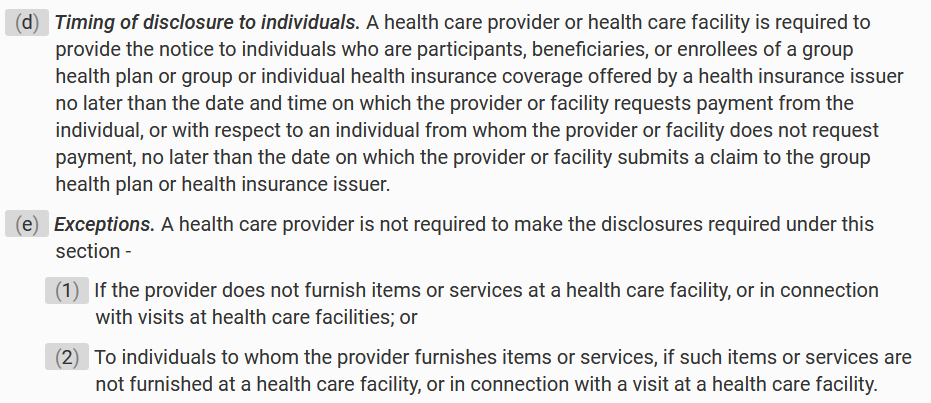
A | The modifier assignment will be dependent on the site of the polyp being removed. If all polyps removed are in the large intestine and each removed by a different method (i.e., cold biopsy, hot biopsy, snare), append modifier XU. The large intestine starts at the sigmoid colon and ends at the cecum. This is considered one anatomic site. Consider these two scenarios. In this scenario, report 45384 for the hot biopsy of polyp in the transverse colon and 45380 for the cold biopsy removal of a polyp in the descending colon. Append modifier XU to 45380 for overlapping services. Although the polyps are identified at different areas of the large intestine, they were in the same anatomic site. The services are considered overlapping since the polyps were removed in different methods (i.e., cold biopsy and hot biopsy). Scenario 2: In this scenario, report 45384 for the hot biopsy of polyp in the transverse colon and 45380 for the cold biopsy removal of a polyp in the rectum. Append modifier XS to 45380 for separate anatomic site. One polyp was identified in the large intestine and the other polyp was in the rectum. Since the rectum is a different anatomic site from the large intestine, XS is appropriate. | |||||||||||||||||||||||||||
Q | We have been holding bills at our Rural Health Clinic for pre-operative clearance visits for Medicare patients scheduled for a colonoscopy. I have been asked to investigate whether these encounters are billable. We have heard that E/Ms “before/prior to” a screening C-scope were not to be billed. However, for the 16 years I have been in clinic billing we have always billed them if they weren’t the “day before or day of” of procedure, as those would get bundled. We’ve gotten paid just fine and in all those years to my knowledge, none of our MC audits resulted in any take backs or fines regarding our billing them. We researched coding forums on-line as well, and any data I could find from or regarding MC and screening C-scopes and opinion, is divided. Many stated that the “before/prior to” means within 24 hours of the procedure; and that they have billed for them as a rule and always been paid (as we did). Others said they felt that the “before/prior to” meant any time, even weeks before, and they didn’t bill for them. Is the “consulting/decision for surgery” visit to a specialist for a screening colonoscopy billable? Also, if the consult/decision for surgery is indeed billable, does it fall into the “day before/day of “rule where it’s not billable even with modifier 57, due to being a minor procedure, or is that rule only regarding pre-ops? Typically, our consults are done days to weeks prior to the scope, but sometimes it is more of a list-minute decision. | |||||||||||||||||||||||||||
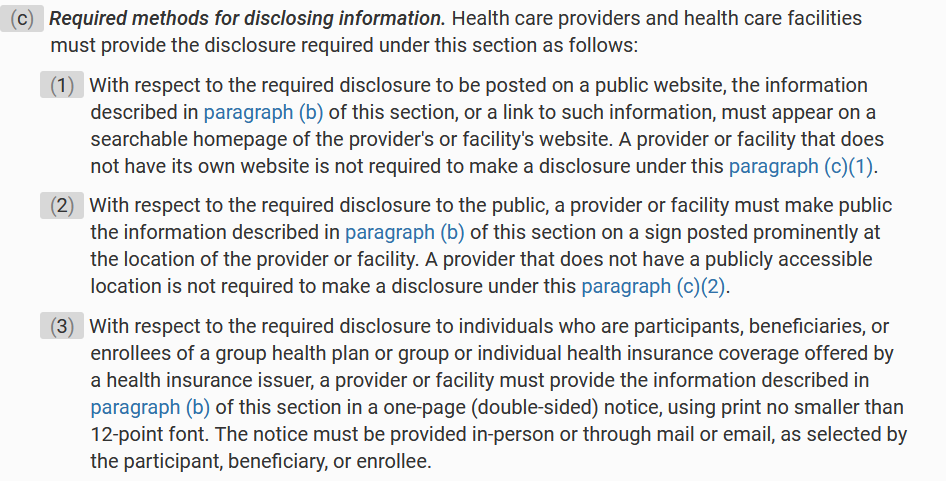
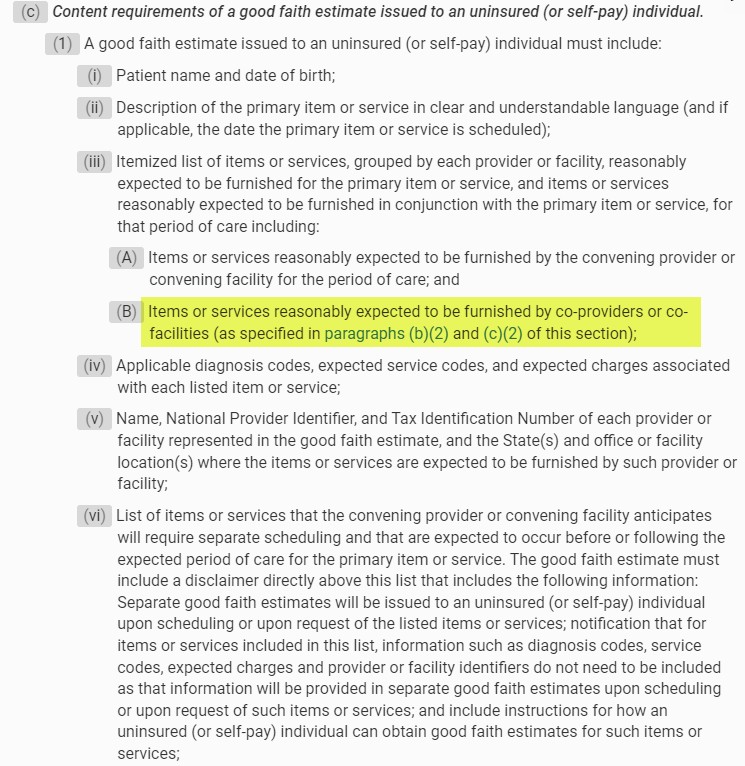
A | Medicare and most other insurers cover only medically necessary services. A patient is eligible for a screening colonoscopy if there are no signs or symptoms of GI trouble. It stands to reason that a pre-op clearance exam that finds no health care condition to support the medical necessity of the visit is not medically necessary, and therefore should not be billed, regardless of the timing (same day or not.) Medicare may have paid claims for such visits at the RHC in the past, but that doesn’t necessarily mean the visits have truly met the general test of medical necessity. However, if there is a medically necessary reason for the visit, such as any other complicating condition that would be pertinent to the safety of the patient while undergoing the procedure (high blood pressure, diabetes, etc.), then the visit might be considered medically necessary. Medical necessity will be determined by the documentation and diagnosis coding provided in addition to the ICD10 Z01.81x (Encounter for preprocedural examinations.) The American Gastroenterological Association website also discusses this issue. If the service is not a screening colonoscopy, then several other factors influence whether a pre-operative H&P visit should be separately reported and/or reimbursed:
As you may already be aware, Medicare assigns a “global” period indicator of 000 to most colonoscopy codes − “000” − Endoscopic or minor procedure with related preoperative and postoperative relative values on the day of the procedure only included in the fee schedule payment amount; evaluation and management services on the day of the procedure generally not payable.” Surgeons may bill for a visit prior to surgery, as they need to evaluate the problem and determine the best surgical approach, but:
Another physician (not the surgeon) can bill for an H&P after the surgeon makes the decision to perform surgery, and refers the patient to a second physician (often a primary care physician) for a preoperative H&P. This service is reportable, but if the visit is not deemed to be medically necessary, a payor may deny payment. Medical necessity will be determined by the documentation and diagnosis coding provided in addition to the ICD10 Z01.81x: ICD-10 Codes
The following matric was created to help simplify the various scenarios when a medically necessary pre-op exam would be billable:
| |||||||||||||||||||||||||||
ParaRev can help
Proper coding and subsequent denials continue to be a challenge as hospitals and healthcare systems struggle with maintaining qualified personal, decreasing margins, and constantly changing requirements. A 2021 audit found that the average accuracy rate for E/M coding was just 81% for hospital billing and 75.3% for professional billing.[1] Regarding denials, hospital billing had an average initial denial rate of 34% while professional billing experienced a 15% rate.[2] In addition, missing modifiers could result in the loss on average of $170 (Professional claim), $690 (hospital outpatient claim), and $900 (hospital outpatient claim).[3]
ParaRev specializes in accounts receivable recovery and resolution and serves as a virtual extension of your hospital’s central billing office to help you quickly resolve and collect more of your insurance accounts receivable. The constantly changing codes and billing requirements can be hard to manage with finite resources. ParaRev’s Data Team can help ensure that changes are implemented in timely and accurately.
Contact ParaRev to learn more about how we can help you improve your hospital’s accounts receivable management.
- Healthcare Auditing and Revenue Integrity: 2021 Benchmarking and Trends Report. Hayes Management.
- Ibid.
- Ibid.

Want to avoid 90% of your hospital denials? Learn 7 strategies to improve your AR.